How I Turned Medical Bills into Smart Investments — A Real Strategy
What if your medical expenses could actually help grow your wealth instead of draining it? That’s exactly what I discovered after facing unexpected health costs. Instead of just paying and moving on, I used strategic financial planning to turn those moments into opportunities. It wasn’t easy, but by focusing on long-term gains and risk control, I built a system that protects my health — and my portfolio. This is how I did it, and how you might too.
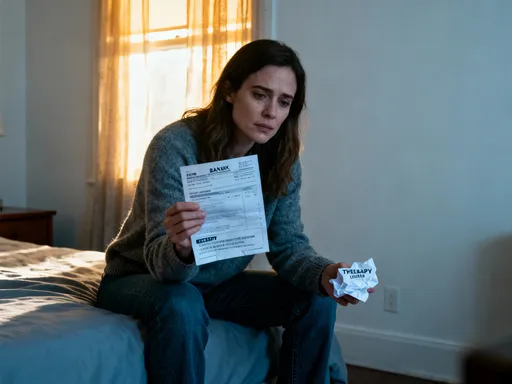
The Hidden Cost of Healthcare (And the Opportunity Within)
Medical expenses are often seen as a financial black hole — a place where money goes in and nothing comes out. But this view overlooks a powerful truth: every health-related expense can serve as a catalyst for smarter financial behavior. When approached with foresight, medical spending doesn’t have to be purely reactive. It can become the starting point for a more resilient financial life. Many people only think about money during a crisis, but those moments can reveal gaps in planning that, once addressed, lead to stronger long-term outcomes.
Consider the case of a woman in her early 50s who faced a surprise diagnosis requiring surgery. The initial bill was over $15,000 after insurance. Rather than seeing it as a setback, she used the experience to reevaluate her entire financial picture. She discovered she had been paying for a low-deductible insurance plan with high premiums — a structure that made sense in her 30s but no longer fit her current health and income level. By switching to a high-deductible health plan and opening a Health Savings Account (HSA), she not only reduced her monthly costs but began building tax-free savings she could invest. This shift didn’t erase the bill, but it transformed how she would handle future expenses.
The opportunity within medical costs lies in forced reflection. A major bill disrupts routine, creating a moment to ask: Are my current financial tools working for me? Am I protected against future shocks? Is there a smarter way to manage healthcare spending? These questions, when answered proactively, can lead to decisions that generate long-term value. For example, using medical expenses to justify opening an HSA isn’t just about covering costs — it’s about unlocking tax advantages and investment growth that continue long after the check is written.
Moreover, the emotional weight of a health crisis often leads to impulsive financial choices — like putting bills on high-interest credit cards or withdrawing from retirement accounts. But with a structured approach, those same pressures can instead push individuals toward better habits. The key is to treat each medical expense not as an isolated event, but as a signal. It signals the need for better planning, smarter insurance choices, and more intentional saving. When viewed this way, even a painful bill becomes a valuable piece of financial feedback.
Building a Financial Shield: Health Savings That Work Harder
Not all savings accounts are created equal, and nowhere is this more evident than in how they handle healthcare costs. Traditional savings accounts earn minimal interest and offer no tax benefits, making them inefficient tools for managing medical expenses. But specialized accounts like Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) are designed to do more than just store money — they help it grow while reducing tax liability. For individuals with qualifying high-deductible health plans, an HSA is one of the most powerful financial tools available, offering triple tax advantages: contributions are tax-deductible, earnings grow tax-free, and withdrawals for qualified medical expenses are also tax-free.
What makes an HSA truly unique is its flexibility over time. Unlike an FSA, which typically requires you to use the money within a calendar year or lose it, HSA funds roll over indefinitely. This means you can contribute during healthy years, let the balance grow through investment options, and withdraw decades later for future medical needs — including long-term care or retirement-era expenses. Some financial institutions even allow HSA holders to invest their balances in mutual funds or index funds, turning what starts as a savings vehicle into a long-term investment account.
The real power of these accounts becomes clear when used strategically. Imagine a 45-year-old woman who contributes $3,000 annually to her HSA and invests the funds in a diversified portfolio earning an average of 6% per year. After 20 years, her account could grow to over $110,000 — all tax-free when used for medical purposes. Even better, after age 65, she can withdraw funds for any reason without penalty (though non-medical withdrawals are taxed as income). This dual-purpose design makes the HSA not just a health tool, but a retirement planning asset.
Yet many eligible individuals never open an HSA, either because they don’t understand the benefits or assume they can’t afford to contribute. The truth is, even small, consistent contributions can yield significant results over time. The key is to treat HSA funding as a priority, not an afterthought. By redirecting money that would otherwise go toward premiums in a traditional plan, or by automating monthly deposits, individuals can build a financial shield that works harder than passive savings ever could. In this way, medical expenses aren’t just covered — they’re anticipated, managed, and even leveraged for growth.
When Medical Debt Becomes a Wealth Warning Sign
Medical debt is one of the leading causes of financial distress in households, but it’s rarely the result of a single catastrophic bill. More often, it stems from a series of small missteps — delayed insurance claims, misunderstood billing codes, or payment plans with hidden interest. These seemingly minor oversights can compound into long-term financial strain, turning a manageable expense into a persistent burden. However, rather than viewing medical debt as a failure, it’s more productive to see it as a warning sign — a signal that current financial systems are not equipped to handle health-related risks.
One common trap is the use of hospital-sponsored payment plans that appear interest-free but carry high effective rates if not managed carefully. For example, a patient may agree to pay $500 per month for 12 months on a $6,000 bill, only to find that missing one payment triggers retroactive interest on the entire balance. These terms are often buried in fine print, and without careful review, patients can end up paying thousands more than expected. Another frequent issue is the delay in filing insurance claims, which can result in denied coverage and full out-of-pocket responsibility. These are not signs of personal failure, but of a complex system that rewards financial literacy and punishes oversight.
The good news is that recognizing these patterns early allows for course correction. A woman in her late 40s realized she had accumulated $8,000 in medical debt not from one procedure, but from three separate bills she had put on credit cards while waiting for insurance reimbursement. Once she audited her statements, she discovered two claims had been denied due to missing documentation — a fixable issue. By resubmitting the paperwork and negotiating the remaining balance, she reduced her debt by nearly 40%. She then set up a dedicated folder for all medical records and created a calendar reminder to follow up on claims within 30 days of service.
This kind of proactive management transforms debt from a source of shame into a learning opportunity. It highlights the importance of documentation, timely follow-up, and understanding the terms of every financial agreement. More importantly, it underscores the need for a buffer — whether an emergency fund or a credit line with favorable terms — to avoid relying on high-cost options during uncertain periods. When medical debt appears, it’s not just a reminder to pay a bill; it’s a signal to strengthen financial systems, improve oversight, and build resilience against future shocks.
Investing in Prevention: The Highest-Return Healthcare Move
If there were a financial investment guaranteed to deliver double-digit returns, everyone would want in. Yet one of the highest-return strategies available — preventive healthcare — is consistently underfunded and undervalued. Routine screenings, vaccinations, fitness programs, and nutritional improvements may seem like small expenses, but they can prevent far larger costs down the road. Studies show that every dollar spent on preventive care can save up to $5.80 in future medical expenses, particularly for chronic conditions like diabetes, heart disease, and certain cancers. For a family managing long-term health, these savings are not just theoretical — they are measurable and life-changing.
Consider the case of a woman who began experiencing mild hypertension in her mid-50s. Instead of waiting for a crisis, she invested in a year-long wellness program that included regular blood pressure monitoring, dietary coaching, and a gym membership. The total cost was around $1,200. Within nine months, her blood pressure normalized, and she avoided the need for prescription medication — which would have cost over $600 per year, not including doctor visits and potential side effects. More importantly, she reduced her risk of stroke and heart attack, conditions that carry average treatment costs of over $100,000. Her upfront spending wasn’t an expense — it was a high-yield investment in her future health and financial stability.
Prevention extends beyond clinical care. Lifestyle choices — such as maintaining a healthy weight, avoiding smoking, and managing stress — have profound financial implications. A person who exercises regularly and eats a balanced diet is less likely to develop chronic illnesses, miss work, or require expensive interventions. These benefits compound over time, preserving both quality of life and financial resources. Employers recognize this, which is why many offer wellness incentives, gym reimbursements, or discounted insurance premiums for healthy behaviors. Individuals can adopt the same logic by treating health as an asset to be maintained, not a problem to be fixed.
The mindset shift is critical: instead of seeing preventive care as an optional cost, it should be viewed as essential maintenance — like servicing a car before the engine fails. Delaying a mammogram to save $200 might seem prudent in the short term, but if a condition goes undetected, the long-term costs can be devastating. By prioritizing prevention, individuals gain control over their health trajectory and reduce the likelihood of sudden, disruptive expenses. This approach doesn’t eliminate all risk, but it dramatically improves the odds of avoiding the most costly outcomes. In financial terms, that’s the definition of risk management.
Aligning Insurance with Investment Goals
Health insurance is often chosen based on immediate cost — the lowest premium wins. But this short-term thinking can undermine long-term financial goals. The right insurance plan doesn’t just minimize today’s payment; it supports tomorrow’s growth. For many individuals, especially those with stable health and access to an HSA, a high-deductible health plan (HDHP) offers a strategic advantage. While the deductible is higher, the lower monthly premiums free up cash flow that can be redirected into savings or investments. When paired with an HSA, this structure creates a powerful synergy: reduced expenses now, tax-advantaged growth later.
Take the example of a couple in their early 50s who switched from a traditional PPO plan with a $600 monthly premium to an HDHP with a $350 premium. The $250 monthly difference allowed them to contribute $3,000 annually to their HSA — the maximum allowed at the time. Over ten years, even with modest investment returns, their HSA grew to over $45,000, all tax-free for medical use. They still paid out-of-pocket for routine care, but those costs were predictable and manageable. When an unexpected procedure arose, they used HSA funds instead of dipping into retirement accounts or credit cards. Their insurance didn’t prevent the expense, but their financial strategy prevented the crisis.
Not every plan suits every person, of course. Families with frequent medical needs may benefit more from lower deductibles and broader coverage, even at higher premiums. The key is alignment — matching insurance choices to personal health patterns, financial capacity, and long-term goals. A young parent managing a child’s asthma will have different priorities than a healthy retiree focused on minimizing taxes. What matters is intentionality: selecting a plan not by default, but by design.
Additionally, many people overlook the investment potential of their insurance decisions. A plan that allows HSA contributions isn’t just cheaper — it’s a gateway to tax-free wealth building. Choosing a plan without this option may save a few dollars today but cost thousands in lost opportunities over time. Reviewing options annually during open enrollment, understanding the full scope of benefits, and projecting costs under different scenarios can lead to smarter, more strategic choices. Insurance, when viewed through a financial lens, becomes more than protection — it becomes part of a larger wealth strategy.
Turning Medical Setbacks into Portfolio Strength
Financial resilience isn’t measured during calm periods — it’s tested during disruptions. A medical setback can expose weaknesses in a financial plan, but it can also reveal strengths when proper systems are in place. Liquidity, emergency funds, and diversified income streams are not just abstract concepts; they are the tools that allow individuals to absorb shocks without derailing long-term goals. A well-prepared investor doesn’t avoid medical costs — they plan for them, ensuring that a health crisis doesn’t force the sale of assets at a loss or the abandonment of retirement timelines.
Scenario modeling shows how different levels of preparedness lead to vastly different outcomes. Consider two individuals facing the same $10,000 medical bill. One has no emergency fund and relies on credit cards with a 19% interest rate. Over five years, that debt could cost over $13,000 in total payments. The other has a fully funded emergency account and pays in full, preserving credit and avoiding interest. The financial difference is clear — but so is the psychological one. The second individual maintains control, while the first feels trapped by mounting payments.
Beyond emergency savings, diversified income sources add another layer of protection. A woman who earns supplemental income through part-time consulting was able to cover a major dental procedure without touching her investments. Meanwhile, her neighbor, reliant solely on a fixed salary, delayed treatment for months due to cash flow concerns. Over time, the untreated issue led to more extensive (and expensive) care. Diversification isn’t just for portfolios — it applies to income as well. Multiple streams increase flexibility, allowing individuals to handle unexpected costs without sacrificing long-term growth.
Interestingly, some investors have even used medical challenges as opportunities to reassess their portfolios. During a period of forced downtime, one woman reviewed her asset allocation and shifted toward more stable, income-generating investments. The change didn’t erase her health struggle, but it improved her financial footing. Resilience, in this sense, is not about avoiding hardship — it’s about designing a system that withstands it. When health and wealth planning are integrated, setbacks don’t end progress — they refine it.
The Long Game: Health, Wealth, and Smart Trade-Offs
True financial success isn’t about maximizing returns at all costs — it’s about making sustainable, intentional choices that balance immediate needs with future goals. This principle applies powerfully to healthcare spending. Delaying a non-essential cosmetic procedure to fund an HSA contribution, choosing generic prescriptions when appropriate, or opting for in-network providers are not acts of deprivation — they are examples of smart trade-offs. These decisions free up capital that can be redirected toward investments with compounding benefits, such as retirement accounts, education funds, or home equity.
The mindset shift required is subtle but profound: health and wealth are not competing priorities — they are interconnected assets. A dollar spent wisely on prevention today can save thousands tomorrow. A premium reduced by choosing the right insurance plan can fund years of tax-advantaged growth. A medical bill, instead of being a source of stress, can become a catalyst for better planning. This is not about cutting corners or avoiding care — it’s about optimizing choices to support long-term well-being.
Discipline and foresight are the cornerstones of this approach. It requires tracking expenses, understanding benefits, and making decisions based on data rather than emotion. It means setting up systems — automatic HSA contributions, claim tracking calendars, preventive care schedules — that reduce the cognitive load of financial management. And it involves regular review, adjusting strategies as health, income, and life circumstances change.
Ultimately, the goal is not to eliminate medical spending — that’s impossible and unwise. The goal is to master the financial wisdom behind it. By treating healthcare as a predictable, manageable part of life — not a crisis to be feared — individuals gain power over their financial destiny. They stop reacting and start planning. They stop losing and start growing. And in the process, they turn one of life’s greatest uncertainties into a force for lasting gain.